Coronavirus Disease 2019 (COVID-19) is a respiratory disease caused by the SARS-CoV-2 virus. It has spread from China to many other countries around the world. To reduce the impact of COVID-19 outbreak conditions on businesses, workers, customers, and the public, it is important for all employers to plan now for COVID-19. The Occupational Safety and Health Administration (OSHA) developed this COVID-19 planning guidance based on traditional infection prevention and industrial hygiene practices. It focuses on the need for employers to implement engineering, administrative, and work practice controls and personal protective equipment (PPE), as well as considerations for doing so.
How COVID-19 Spreads
The virus is thought to spread mainly from person- to-person, including:
- Between people who are in close contact with one another (within about 6 feet).
- Through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
It may be possible that a person can get COVID-19 by touching a surface or object that has SARS-CoV-2 on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the primary way the virus spreads. People are thought to be most contagious when they are most symptomatic (i.e., experiencing fever, cough, and/or shortness of breath). Some spread might be possible before people show symptoms; there have been reports of this type of asymptomatic transmission with this new coronavirus, but this is also not thought to be the main way the virus spreads.
Classifying Worker Exposure to SARS-CoV-2
Worker risk of occupational exposure to SARS-CoV-2, the virus that causes COVID-19, during an outbreak may vary from very high to high, medium, or lower (caution) risk. The level of risk depends in part on the industry type, need for contact within 6 feet of people known to be, or suspected of being, infected with SARS-CoV-2, or requirement for repeated or extended contact with persons known to be, or suspected of being, infected with SARS-CoV-2. To help employers determine appropriate precautions, OSHA has divided job tasks into four risk exposure levels: very high, high, medium, and lower risk. The Occupational Risk Pyramid shows the four exposure risk levels in the shape of a pyramid to represent probable distribution of risk:
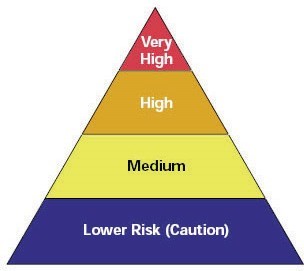
Considering the nature of work and taking a conservative approach, we took the liberty in considering the construction industry as a Medium Exposure Risk level. Medium exposure risk jobs include those that require frequent and/or close contact with (i.e., within 6 feet of) people who may be infected with SARS-CoV-2, but who are not known or suspected COVID-19 patients. In areas without ongoing community transmission, workers in this risk group may have frequent contact with travelers who may return from international locations with widespread COVID-19 transmission. In areas where there is ongoing community transmission, workers in this category may have contact with the general public (e.g., schools, high-population-density work environments, some high-volume retail settings).
What to Do to Protect Workers – Pre-requisite
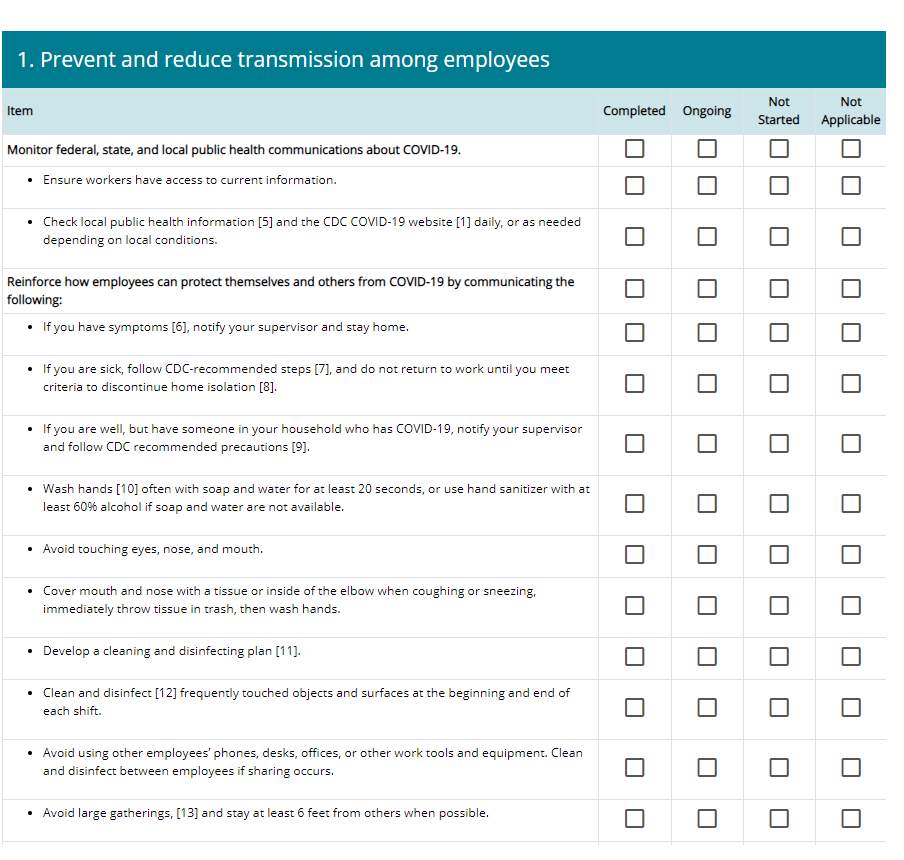
The CDC has developed a Resuming Business Toolkit to assist employers in slowing the spread of COVID-19 and lowering the impact in their workplace when reintegrating employees into non-healthcare business settings. One of the resources in this toolkit is the Restart Readiness Checklist
1) Develop an Infectious Disease Preparedness and Response Plan
If one does not already exist, develop an infectious disease preparedness and response plan that can help guide protective actions against COVID-19.
Stay abreast of guidance from federal, state, local, tribal, and/or territorial health agencies, and consider how to incorporate those recommendations and resources into workplace-specific plans.
Plans should consider and address the level(s) of risk associated with various worksites and job tasks workers perform at those sites. Such considerations may include:
- Where, how, and to what sources of SARS-CoV-2 might workers be exposed, including: The general public, customers, and coworkers; and Sick individuals or those at particularly high risk of infection (e.g., international travelers who have visited locations with widespread sustained (ongoing) COVID-19 transmission, healthcare workers who have had unprotected exposures to people known to have, or suspected of having, COVID-19).
- Non-occupational risk factors at home and in community settings.
- Workers’ individual risk factors (e.g., older age; presence of chronic medical conditions, including immuno-compromising conditions; pregnancy).
- The need for social distancing, staggered work shifts, downsizing operations, delivering services remotely, and other exposure-reducing
- Options for conducting essential operations with a reduced workforce, including cross-training workers across different jobs in order to continue operations or deliver surge
2) Prepare to Implement Basic Infection Prevention Measures
For most employers, protecting workers will depend on emphasizing basic infection prevention measures. As appropriate, all employers should implement good hygiene and infection control practices, including:
- Improving the building ventilation system
- Promote frequent and thorough hand washing, including by providing workers, customers, and worksite visitors with a place to wash their hands. If soap and running water are not immediately available, provide alcohol-based hand rubs containing at least 60%
- Encourage workers to stay home if they are sick.
- Encourage respiratory etiquette, including covering coughs and
- Provide customers and the public with tissues and trash receptacles.
- Employers should explore whether they can establish policies and practices, such as flexible worksites (e.g., telecommuting) and flexible work hours (e.g., staggered shifts), to increase the physical distance among employees and between employees and others if state and local health authorities recommend the use of social distancing
- Discourage workers from using other workers’ phones, desks, offices, or other work tools and equipment, when
- Maintain regular housekeeping practices, including routine cleaning and disinfecting of surfaces, equipment, and other elements of the work environment. When choosing cleaning chemicals, employers should consult information on your local Environmental Agency -approved disinfectant labels with claims against emerging viral pathogens. Products with approved emerging viral pathogens claims are expected to be effective against SARS-CoV-2 based on data for harder to kill viruses. F
3) Develop Policies and Procedures for Prompt Identification and Isolation of Sick People, if Appropriate
- Prompt identification and isolation of potentially infectious individuals is a critical step in protecting workers, customers, visitors, and others at a
- Employers should inform and encourage employees to self-monitor for signs and symptoms of COVID-19 if they suspect possible exposure.
- Employers should develop policies and procedures for employees to report when they are sick or experiencing symptoms of COVID-19.
- Where appropriate, employers should develop policies and procedures for immediately isolating people who have signs and/or symptoms of COVID-19, and train workers to implement them. Move potentially infectious people to a location away from workers, customers, and other visitors. Although most worksites do not have specific isolation rooms, designated areas with closable doors may serve as isolation rooms until potentially sick people can be removed from the worksite.
- Take steps to limit spread of the respiratory secretions of a person who may have COVID-19. Provide a face mask, if feasible and available, and ask the person to wear it, if tolerated. Note: A face mask (also called a surgical mask, procedure mask, or other similar terms) on a patient or other sick person should not be confused with PPE for a worker; the mask acts to contain potentially infectious respiratory secretions at the source (i.e., the person’s nose and mouth).
- If possible, isolate people suspected of having COVID-19 separately from those with confirmed cases of the virus to prevent further transmission—particularly in worksites where medical screening, triage, or healthcare activities occur, using either permanent (e.g., wall/different room) or temporary barrier (e.g., plastic sheeting).
- Restrict the number of personnel entering isolation
- Protect workers in close contact with (i.e., within 6 feet of) a sick person or who have prolonged/repeated contact with such persons by using additional engineering and administrative controls, safe work practices, and PPE. Workers whose activities involve close or prolonged/ repeated contact with sick people are addressed further in later sections covering workplaces classified at medium and very high or high exposure risk.
4) Develop, Implement, and Communicate about Workplace Flexibilities and Protections
- Actively encourage sick employees to stay in isolation
- Ensure that sick leave policies are consistent with public health guidance and that employees are aware of these
- Talk with companies that provide your business with contract or temporary employees about the importance of sick employees staying home and encourage them to develop non-punitive leave
- Do not require a healthcare provider’s note for employees who are sick with acute respiratory illness to validate their illness or to return to work, as healthcare provider offices and medical facilities may be extremely busy and not able to provide such documentation in a timely
- Provide adequate, usable, and appropriate training, education, and informational material about business-essential job functions and worker health and safety, including proper hygiene practices and the use of any workplace controls (including PPE).
“Informed workers who feel safe at work are less likely to be unnecessarily absent.”


Implement Workplace Controls
During a COVID-19 outbreak, when it may not be possible to eliminate the hazard, the most effective protection measures are (listed from most effective to least effective): engineering controls, administrative controls, safe work practices (a type of administrative control), and PPE. There are advantages and disadvantages to each type of control measure when considering the ease of implementation, effectiveness, and cost. In most cases, a combination of control measures will be necessary to protect workers from exposure to SARS-CoV-2.
In addition to the types of workplace controls discussed below, CDC guidance for businesses provides employers and workers with recommended SARS-CoV-2 infection prevention strategies to implement in workplaces: www.cdc.gov/coronavirus/2019- ncov/specific-groups/guidance-business-response.html.
1) Engineering Controls
Engineering controls involve isolating employees from work- related hazards. In workplaces where they are appropriate, these types of controls reduce exposure to hazards without relying on worker behavior and can be the most cost-effective solution to implement. Engineering controls for SARS-CoV-2 include:
- Installing high-efficiency air
- Increasing ventilation rates in the work
- Installing physical barriers, such as clear plastic sneeze
- Specialized negative pressure ventilation in some settings, such as for aerosol generating procedures (e.g., airborne infection isolation rooms in healthcare settings and specialized autopsy suites in mortuary settings).
- Alter the workspace to maintain social distancing. Examples include: arrange partitions as a barrier shield, move electronic payment reader away from cashier, use verbal announcements, signs, and visual cues to promote social distancing. remove/rearrange furniture, provide remote delivery alternatives.
2) Administrative Controls
Administrative controls require action by the worker or employer. Typically, administrative controls are changes in work policy or procedures to reduce or minimize exposure to a hazard. Examples of administrative controls for SARS-CoV-2 include:
- Encouraging sick workers to stay at home
- Consider conducting daily in-person or virtual health checks (e.g., symptom and/or temperature screening) before employees enter the facility.
- Minimizing contact among workers, clients, and customers by replacing face-to-face meetings with virtual communications and implementing telework
- Establishing alternating days or extra shifts that reduce the total number of employees in a facility at a given time, allowing them to maintain distance from one another while maintaining a full onsite work week.
- Restrict access to reduce the number of workers in enclosed and confined areas at one time. Confined and enclosed areas (e.g., trailers, small rooms in buildings under construction) should be identified and access should be restricted to essential personnel only. Enclosed spaces (e.g., toilets, break areas) are potential transmission areas and should be treated accordingly. Time spent in these areas should be minimized.
- Remove or rearrange chairs and tables or add visual cue marks in break areas to support social distancing practices between workers. Identify alternative areas to accommodate overflow volume.
- Discontinuing nonessential travel to locations with ongoing COVID-19 Regularly check CDC travel warning levels
- Replace high-touch communal items, such as coffee pots, water coolers, and bulk snacks, with alternatives such as pre-packaged, single-serving items.
- Developing emergency communications plans, including a forum for answering workers’ concerns and internet-based communications
- Providing workers with up-to-date education and training on COVID-19 risk factors and protective behaviors (e.g., cough etiquette and care of PPE).
- Training workers who need to use protecting clothing and equipment how to put it on, use/wear it, and take it off correctly, including in the context of their current and potential duties. Training material should be easy to understand and available in the appropriate language and literacy level for all workers.
- Consider offering face masks and event of a shortage of masks, a reusable face shield that can be decontaminated may be an acceptable method of protecting against droplet transmission.
- Where appropriate, limit customers’ and the public’s access to the worksite, or restrict access to only certain workplace
- Consider strategies to minimize face-to-face contact (e.g., drive- through windows, phone-based communication, telework).
- Routinely clean all frequently touched surfaces in the workplace, such as workstations, keyboards, telephones, handrails, printer/copiers, drinking fountains, and doorknobs.
- Provide adequate PPE: Workers with medium exposure risk may need to wear some combination of gloves, a gown, a face mask, and/or a face shield
or goggles. Read 4) below.
3) Safe Work Practices
Safe work practices are types of administrative controls that include procedures for safe and proper work used to reduce the duration, frequency, or intensity of exposure to a hazard. Examples of safe work practices for SARS-CoV-2 include:
- Designate a safety and health officer to be responsible for responding to COVID-19 concerns at every jobsite. Workers should know who this person is and how to contact them.
- Providing resources and a work environment that promotes personal hygiene. For example, provide tissues, no-touch trash cans, hand soap, alcohol-based hand rubs containing at least 60 percent alcohol, disinfectants, and disposable towels for workers to clean their work
- Requiring regular hand washing or using of alcohol-based hand rubs. Workers should always wash hands when they are visibly soiled and after removing any
- Post handwashing signs in bathrooms and pantries, cafeterias.
- Limit tool sharing if possible.
- Practice proper hand hygiene. This is an important infection control measure. With appropriate hand hygiene, you do not need gloves to protect you from COVID-19. When possible, wash your hands regularly with soap and water for at least 20 seconds or use an alcohol-based hand sanitizer containing at least 60% alcohol. Key times to clean hands include:
- Before and after work shifts and breaks
- After blowing your nose, coughing, or sneezing
- After using the restroom
- Before eating and before and after preparing food
- After touching objects which have been handled by coworkers, such as tools and equipment
- Before putting on and after taking off work gloves
- After putting on, touching, or removing cloth face coverings
- Before donning or doffing eye or face protection (safety glasses, goggles, etc.)
- Do not touch your eyes, nose, or mouth.
- Use tissues when you cough, sneeze, or touch your face. Throw used tissues in the trash and wash your hands or use hand sanitizer containing 60% alcohol if a sink to wash your hands is not available.
- Provide a large (5+ gallon) bucket with a lid and tap that can be used to provide water for handwashing. If this method is used, the water tap should be regularly cleaned and disinfected, and the contaminated wastewater must be collected and treated in accordance with local laws and environmental regulations. Provide fresh clean water daily.
- Depending on the size or configuration of the job site, there may need to be multiple handwashing stations available to accommodate the workforce while maintaining social distancing, and stations may need to be restocked during the course of the day to maintain adequate handwashing supplies.
4) Personal Protective Equipment (PPE)
While engineering and administrative controls are considered more effective in minimizing exposure to SARS-CoV-2, employers are obligated to provide their workers with PPE. While correctly using PPE can help prevent some exposures, it should not take the place of other prevention strategies.
Examples of PPE include: gloves, goggles, face shields, face masks, and respiratory protection, when appropriate. During an outbreak of an infectious disease, such as COVID-19, recommendations for PPE specific to occupations or job tasks may change depending on geographic location, updated risk assessments for workers, and information on PPE effectiveness in preventing the spread of COVID-19. All types of PPE must be:
- Selected based upon the hazard to the worker.
- Properly fitted and periodically refitted, as applicable (e.g., respirators).
- Consistently and properly worn when required.
- Regularly inspected, maintained, and replaced, as necessary.
- Properly removed, cleaned, and stored or disposed of, as applicable, to avoid contamination of self, others, or the environment.

How to Contact OSHA
Under the Occupational Safety and Health Act of 1970, employers are responsible for providing safe and healthful workplaces for their employees. OSHA’s role is to help ensure these conditions, and providing training, education and assistance. For more information, visit www.osha.gov

End.
Sources:
https://www.cdc.gov/coronavirus/2019-ncov/community/
